Bleeding Menstrual: What is Normal and What is Abnormal
Bleeding Menstrual: What is Normal and What is Abnormal
Menstrual bleeding, or menstruation, is a complex physiological process that involves the shedding of the endometrial lining of the uterus. This guide, formulated with insights from Dr. Hema Jonnalagadda, aims to provide an exhaustive, scientifically detailed overview of normal and abnormal menstrual bleeding. This resource will address every aspect of menstrual health, offering comprehensive knowledge to clarify all potential queries.
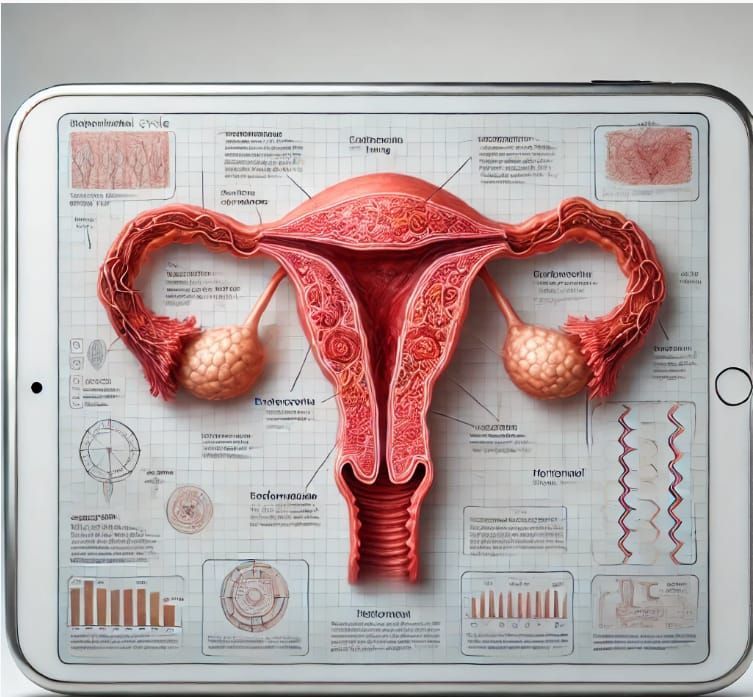

Menstrual Cycle Phases: A Detailed Breakdown with Simplified Clarifications
The menstrual cycle is regulated by a finely tuned interplay of hormones. It is typically divided into four phases:
Menstrual Phase (Days 1-5)
● Pathophysiology: Shedding of the functional layer of the endometrium due to the drop in progesterone levels.
- Simplified Clarification: The uterine lining breaks down and is expelled as menstrual blood due to lower hormone levels.
● Normal Findings: Bleeding lasting 3-7 days with a total blood loss of 30-80 milliliters.
- Simplified Clarification: Menstruation typically lasts 3-7 days, with an average blood loss of 2-6 tablespoons.
Follicular Phase (Days 1-13)
● Endocrine Regulation: Increased secretion of Follicle Stimulating Hormone (FSH) from the anterior pituitary stimulates follicular growth.
- Simplified Clarification: The brain signals the ovaries to start maturing eggs.
● Endometrial Changes: Proliferation of the endometrium due to rising estrogen levels.
- Simplified Clarification: The uterine lining thickens and rebuilds.
Ovulation (Day 14)
● Hormonal Surge: A peak in Luteinizing Hormone (LH) triggers the release of a mature oocyte.
- Simplified Clarification: A spike in a specific hormone causes an egg to be released from the ovary.
● Clinical Significance: Mid-cycle pain (Mittelschmerz) may be observed, and cervical mucus becomes more elastic and clear, facilitating sperm entry.
- Simplified Clarification: Some women feel slight pain during ovulation, and cervical mucus changes to help sperm reach the egg.
Luteal Phase (Days 15-28)
● Hormonal Influence: The corpus luteum secretes progesterone, stabilizing the endometrial lining for potential implantation.
- Simplified Clarification: The body produces a hormone to keep the uterine lining ready for a potential pregnancy.
● Endometrial Maturation: Glandular secretion and increased vascularization of the endometrium.
- Simplified Clarification: The uterine lining becomes nutrient-rich and full of blood vessels to support a possible pregnancy.
Normal Menstrual Bleeding: Clinical and Pathological Insights
Duration and Volume:
● Clinical Norms: Menstrual bleeding lasting between 3-7 days, with an average blood loss of 30-80 milliliters.
● Measurement Techniques: The use of menstrual cups or calibrated sanitary products can aid in quantifying blood loss.

Color and Consistency:
● Hemoglobin Breakdown: Initial bright red bleeding progressing to darker red or brown due to oxidation.
● Clot Formation: Small clots are normal; large clots may indicate excessive bleeding or an underlying coagulopathy.
Cycle Regularity:
● Eumenorrhea: Regular cycles ranging from 21 to 35 days.
● Variations: Minor deviations are normal but should be monitored if consistent irregularities occur.
Abnormal Menstrual Bleeding (AUB): Etiologies and Diagnostics
Abnormal uterine bleeding (AUB) can be a symptom of various underlying pathologies. The International Federation of Gynecology and Obstetrics (FIGO) classifies AUB into structural and non-structural causes using the PALM-COEIN system:
Structural Causes (PALM)
- Polyp : Endometrial or cervical polyps causing irregular bleeding.
- Simplified Clarification : Non-cancerous growths in the uterus or cervix that can cause unusual bleeding.
- Adenomyosis : Invasion of endometrial tissue into the myometrium, resulting in heavy, painful periods.
- Simplified Clarification : When the lining of the uterus grows into the muscle wall, causing heavy and painful periods.
- Leiomyoma (Fibroids) : Benign uterine tumors causing menorrhagia and pressure symptoms.
- Simplified Clarification : Non-cancerous tumors in the uterus that cause heavy bleeding and a feeling of pressure.
- Malignancy and Hyperplasia : Endometrial hyperplasia and cancer presenting with postmenopausal bleeding or irregular heavy bleeding.
- Simplified Clarification : Thickening of the uterine lining or cancer, which can cause unusual heavy bleeding, especially after menopause.
Non-Structural Causes (COEIN)
- Coagulopathy : Conditions such as von Willebrand disease leading to excessive bleeding.
- Simplified Clarification : Blood clotting disorders that cause too much bleeding.
- Ovulatory Dysfunction: Irregular ovulation causing unpredictable bleeding patterns.
- Simplified Clarification : Irregular ovulation leading to unpredictable menstrual cycles.
- Endometrial : Primary endometrial dysfunction without a definable structural cause.
- Simplified Clarification : Issues with the uterine lining that aren't caused by growths or other structural problems.
- Iatrogenic : Medications or devices (e.g., IUDs) leading to abnormal bleeding.
- Simplified Clarification : Certain medications or medical devices can cause unusual bleeding.
- Not Yet Classified : Cases where the etiology remains unclear.
- Simplified Clarification : Causes of abnormal bleeding that haven't been identified yet.
Heavy Menstrual Bleeding (Menorrhagia)
● Pathophysiology: Often due to uterine fibroids, adenomyosis, or coagulopathies.
● Clinical Assessment: Laboratory evaluation (CBC, coagulation profile), imaging (ultrasound, MRI), and endometrial biopsy as needed.
Intermenstrual Bleeding
● Etiologies: Can result from hormonal contraception, infections, or structural abnormalities.
● Diagnostics: Pap smear, pelvic ultrasound, and hysteroscopy.
Postmenopausal Bleeding
● Red Flags: Requires immediate investigation to rule out endometrial carcinoma.
● Investigative Protocols: Transvaginal ultrasound and endometrial biopsy.
Light Menstrual Bleeding (Hypomenorrhea)
● Causes: Hormonal contraception, chronic medical conditions, or Asherman’s syndrome.
● Management: Hormonal assessment, hysteroscopy for intrauterine adhesions.
Infrequent Menstrual Bleeding (Oligomenorrhea)
● Common Causes: PCOS, thyroid dysfunction, hyperprolactinemia.
● Evaluation: Hormonal profile, pelvic ultrasound, and MRI of the pituitary gland if necessary.
Frequent Menstrual Bleeding (Polymenorrhea)
● Considerations: Hormonal imbalances, endometrial pathology.
● Assessment: Endocrine evaluation, endometrial sampling.
Painful Menstrual Bleeding (Dysmenorrhea)
● Primary: Excessive prostaglandin production leading to uterine contractions.
● Secondary: Endometriosis, fibroids, or pelvic inflammatory disease (PID).
● Management: NSAIDs, hormonal treatments, laparoscopic evaluation for endometriosis.
Diagnostic and Therapeutic Approaches
Diagnostic Tools
● Transvaginal Ultrasound: Gold standard for evaluating endometrial and myometrial pathology.
● Saline Infusion Sonography (SIS): Enhances the evaluation of intrauterine pathology.
● MRI: Detailed imaging for complex cases, especially adenomyosis or deep infiltrating endometriosis.
● Hysteroscopy: Direct visualization and biopsy of intrauterine lesions.
● Endometrial Biopsy: Essential for ruling out hyperplasia or malignancy.
Treatment Modalities
● Medical Management:
- Hormonal Therapy: Combined oral contraceptives, progestins, GnRH analogs.
- Non-Hormonal: NSAIDs, antifibrinolytics like tranexamic acid.
● Surgical Interventions:
- Dilation and Curettage (D&C): For diagnostic and therapeutic purposes.
- Endometrial Ablation: Minimally invasive treatment for menorrhagia.
- Myomectomy: Removal of fibroids preserving the uterus.
- Hysterectomy: Definitive treatment for refractory AUB, especially in the context of malignancy.
Lifestyle and Supportive Measures
● Dietary Modifications: Iron-rich diet to combat anemia, balanced nutrition to maintain hormonal balance.
● Exercise: Regular physical activity to manage weight and reduce stress.
● Stress Management: Techniques like mindfulness, yoga, and counseling.

Conclusion
A thorough understanding of normal and abnormal menstrual bleeding patterns is vital for early detection and management of underlying gynecological disorders. This comprehensive guide serves as an exhaustive resource to demystify menstrual health, providing detailed scientific insights and practical approaches to managing various menstrual disorders.
Advocare Montgomery Gynecology, located in Plymouth Meeting, offers comprehensive care for women's health needs. Many procedures for diagnosing and treating menstrual disorders can be conveniently performed in-office, while others may require specialized referrals. Selecting the right practitioner at the right time is crucial for effective treatment. At Advocare Montgomery Gynecology, Dr. Hema Jonnalagadda and her experienced team are dedicated to offering expert, compassionate care tailored to your individual needs.
For personalized medical advice and treatment, consult with Dr. Hema Jonnalagadda and the team at Advocare Montgomery Gynecology. We have the expertise and resources to help you manage your menstrual health with confidence and ease.
For further information or to schedule an appointment, please visit our [website](https://www.advocaremontgomerygyn.com/).
Choose Advocare Montgomery Gynecology for exceptional care and support on your journey to optimal gynecological health.