Pelvic Health Awareness Month: Why Pelvic Health Matters to Women
Understanding Vulvodynia: A Comprehensive Guide to Chronic Vulvar Pain
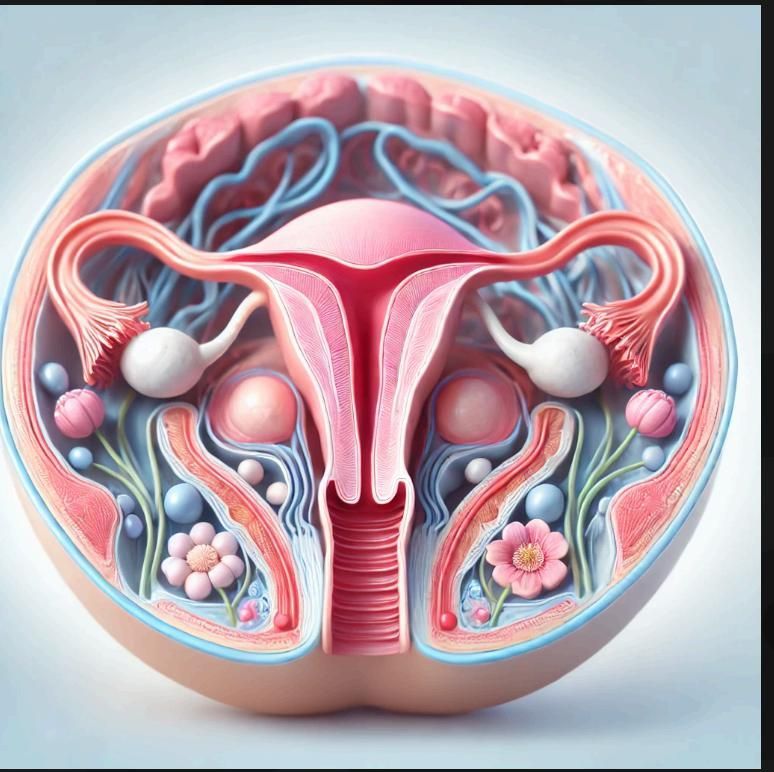
Vulvodynia is a complex, chronic condition that causes unexplained pain in the vulva—the external part of the female genitalia. Affecting approximately 8-16% of women at some point in their lives, vulvodynia is often misunderstood, misdiagnosed, or even ignored, leading many women to suffer in silence. This blog will break down what vulvodynia is, its potential causes, how it’s diagnosed, and the treatment options available. We’ll also look at the latest scientific research to provide a thorough, expert-level understanding of this debilitating condition.
What is Vulvodynia?
Vulvodynia is defined as chronic vulvar pain that lasts for three months or more without an identifiable cause, such as an infection or a skin condition. The pain may be constant or intermittent and can range from mild discomfort to severe, life-altering pain. It can affect daily activities such as sitting, exercising, and sexual intercourse.
There are two primary types of vulvodynia:
● Generalized Vulvodynia: Pain occurs in different areas of the vulva at different times. The discomfort may be constant or occur intermittently and may be triggered by touch or pressure, or occur without a trigger.
● Localized Vulvodynia (Vestibulodynia): Pain is localized to a specific area, usually the vaginal opening. This type is often associated with pain during sexual intercourse, tampon insertion, or gynecological exams

Symptoms of Vulvodynia
The hallmark of vulvodynia is chronic pain in the vulvar region, but the type and intensity of the pain can vary greatly:
● Burning or Stinging Sensation: The most common complaint, described as a persistent or intermittent burning pain.
● Throbbing or Itching: Some women describe their pain as a deep ache or itch.
● Rawness or Soreness: Even light touch, such as wearing tight clothing or sitting, can cause irritation.
● Pain During Sexual Intercourse: This condition can make intimacy extremely painful, leading to emotional and relational strain.
Symptoms may come and go or be constant, and they can appear suddenly or develop gradually.
What Causes Vulvodynia?
The exact cause of vulvodynia remains uncertain, making diagnosis and treatment challenging. However, ongoing research has identified several potential contributors:
1. Nerve Injury or Irritation
One prevailing theory is that vulvodynia is linked to overactivity of the nerves in the vulvar region. In these cases, nerves may send pain signals to the brain even without a specific cause, such as trauma or infection.
2. Chronic Inflammation
Chronic inflammation can affect the tissues of the vulva, leading to ongoing pain. This may stem from repeated infections, allergic reactions, or irritation from hygiene products. However, the inflammation persists even after the initial cause is treated.
3. Hormonal Imbalances
Hormonal changes, particularly reduced estrogen levels, can thin the vulvar tissues, leading to increased sensitivity. This is commonly seen in post-menopausal women but can also occur in younger women due to birth control use or other hormonal changes.
4. Pelvic Floor Muscle Dysfunction
The pelvic floor muscles, which support the bladder, uterus, and rectum, can become tense or dysfunctional, leading to vulvar pain. Women with vulvodynia may experience spasms or tension in these muscles, exacerbating their symptoms.
5. Genetic and Immune Factors
Research suggests that certain women may have a genetic predisposition to vulvodynia. Some studies have found links between vulvodynia and genetic markers related to pain sensitivity. Additionally, abnormalities in the immune response may cause some women to develop the condition after an injury or infection.
6. Central Sensitization
In some cases, women with vulvodynia may have a condition known as central sensitization, where the nervous system becomes hyperactive, making even minor sensations feel painful. This theory suggests that the brain and spinal cord amplify pain signals, turning ordinary sensations like touch or pressure into chronic pain.
How is Vulvodynia Diagnosed?
Diagnosing vulvodynia can be complex, as there is no single test for the condition. Instead, diagnosis is often a process of elimination, ruling out other potential causes of vulvar pain. Here’s how healthcare providers like Dr. Hema Jonnalagadda, M.D., at Advocare Montgomery Gynecology approach the diagnosis:
● Patient History: A detailed history is taken to understand the nature of the pain, its onset, and any associated triggers. Questions may include when the pain began, its intensity, and whether it is constant or intermittent.
● Physical Exam: A pelvic exam is performed to check for other causes of pain, such as infections, skin conditions, or lesions. During the exam, the doctor may use a cotton swab to test different areas of the vulva and vaginal opening for tenderness (called the Q-tip test). This helps identify whether the pain is localized or generalized.
● Lab Tests: Swabs or cultures may be taken to rule out infections like yeast infections or sexually transmitted infections. Blood tests may also be performed to check for hormonal imbalances or inflammatory conditions.
● Pelvic Floor Exam: Given the link between vulvodynia and pelvic floor dysfunction, an internal pelvic floor examination may be done to check for muscle spasms or tightness that could be contributing to the pain.
Treatment Options for Vulvodynia
Treatment for vulvodynia is highly individualized, and a multi-disciplinary approach is often required. The goal is to reduce pain and improve quality of life, and the treatment plan will depend on the underlying cause of the pain.
1. Pelvic Floor Physical Therapy
Pelvic floor dysfunction plays a significant role in many cases of vulvodynia. Pelvic floor physical therapy can help relax and retrain the muscles, reducing pain and discomfort. Techniques may include biofeedback, manual therapy, and relaxation exercises.
2. Medications
- Topical Treatments: Local anesthetics like lidocaine or estrogen creams can provide relief for nerve pain or tissue thinning.
- Oral Medications: Low-dose antidepressants (such as tricyclic antidepressants) or anticonvulsants may be prescribed to calm overactive nerve signals and reduce pain. These medications are particularly helpful for neuropathic pain.
3. Nerve Blocks
For women with severe, persistent pain, nerve blocks can be an effective treatment. These are injections that temporarily block the nerves from sending pain signals to the brain. Nerve blocks can provide relief for weeks or months at a time.
4. Cognitive Behavioral Therapy (CBT)
Because chronic pain often has an emotional and psychological impact, CBT is a valuable tool in managing vulvodynia. It helps women cope with the stress, anxiety, and depression that may accompany long-term pain.
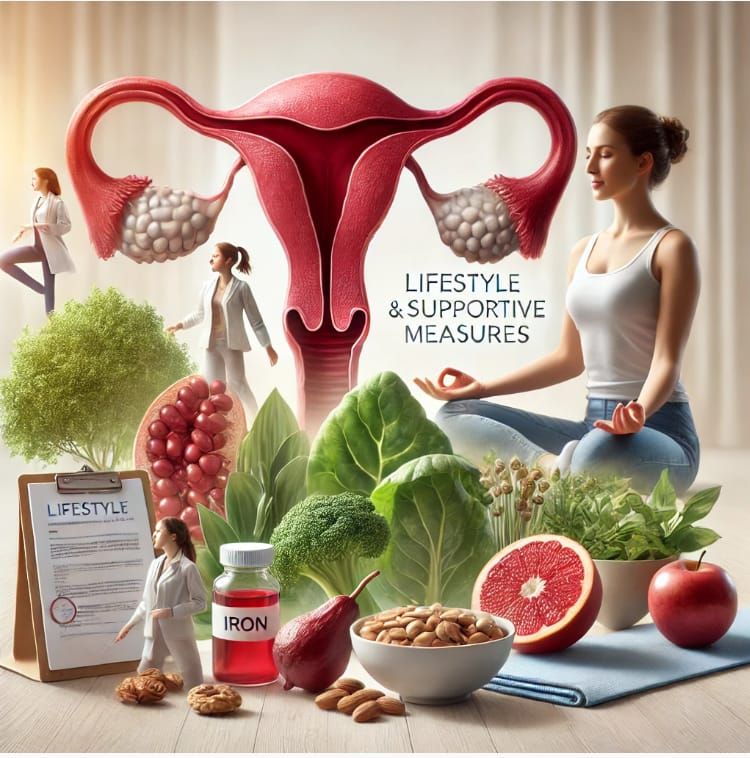
5. Dietary Changes and Supplements
For some women, reducing inflammatory foods or adding supplements like magnesium or omega-3 fatty acids may help reduce pain. However, evidence on the effectiveness of diet in treating vulvodynia is still emerging.
6. Surgery (Vestibulectomy)
In severe cases of localized vulvodynia (vestibulodynia), a surgical procedure called vestibulectomy may be considered. This involves removing the painful tissue from the vestibule (the area around the vaginal opening). Surgery is typically a last resort after other treatments have failed.
The Emotional Impact of Vulvodynia
Living with chronic pain, especially in such a private area, can have profound emotional and psychological effects. Many women with vulvodynia report feelings of isolation, frustration, and depression. The impact on relationships and sexual intimacy can further compound these emotions. It’s essential to seek support—not just medical, but emotional as well.
At Advocare Montgomery Gynecology, we understand that vulvodynia affects more than just physical health. Our comprehensive approach includes counseling and support services to help women manage the emotional toll of this condition.
Take Action: Relief from Vulvodynia is Possible?
Vulvodynia is a complex, often misunderstood condition, but with proper diagnosis and a personalized treatment plan, it is manageable. If you are experiencing persistent vulvar pain, don’t suffer in silence. Dr. Hema Jonnalagadda, M.D., at Advocare Montgomery Gynecology specializes in treating vulvodynia and other complex gynecological conditions. With a compassionate, expert approach, you can regain control of your health and quality of life.
Contact us today to schedule an appointment and start your journey toward relief.