Pelvic Health Awareness Month: Why Pelvic Health Matters to Women
May is Pelvic Health Awareness Month , a time to shine a light on the vital role the pelvis and
pelvic floor play in women’s overall well-being. Pelvic health involves taking care of the muscles
and organs in the lower belly so they function properly and feel good. Yet many women don’t
realize how important pelvic health is until problems arise. In fact, about one in three women will
experience a pelvic health condition at some point in their lives, and these conditions can
significantly impact daily comfort and quality of life. This month (and every month), we aim to
raise awareness, educate, and encourage open conversation about pelvic health
Common Pelvic Health Concerns
Women’s pelvic health can be affected by several common conditions. Here is a brief overview:
● Pelvic Organ Prolapse: This occurs when the muscles and tissues that support pelvic
organs (like the uterus, bladder, or rectum) weaken or loosen. As a result, an organ can
“drop” or press into the vaginal canal. Women with prolapse may feel a bulge or
heaviness in the pelvis, especially during activities or lifting, and sometimes experience
bladder or bowel changes. Many women are embarrassed to discuss these symptoms,
but prolapse is treatable with options like pelvic floor therapy, pessary devices, or
surgery
● Urinary Incontinence: Incontinence is the involuntary leakage of urine, ranging from
occasional drips (for example, when coughing or sneezing) to a sudden strong urge that
can’t be controlled. It affects about one in three women worldwide, often related to
pregnancy, childbirth, or menopause. Importantly, urinary incontinence is not a normal
part of aging and is treatable Treatments include pelvic floor muscle exercises and
other therapies. Early help can prevent it from seriously affecting daily life.
● Endometriosis: Endometriosis happens when tissue like the uterine lining grows
outside the uterus, on ovaries, fallopian tubes, or other pelvic sites This condition
affects roughly 10% of women of reproductive ageIt often causes severe pelvic pain
(especially with periods or intercourse), heavy menstrual bleeding, and sometimes
infertility Endometriosis can lead to chronic inflammation, scar tissue, and painful
adhesions, so early diagnosis and management are crucial.
● Chronic Pelvic Pain: Chronic pelvic pain is ongoing, non-cyclic pain in the pelvis lasting
six months or longer. It can have many causes (or even none clearly identified) and often
coexists with other issues like endometriosis, irritable bowel syndrome, or interstitial
cystitis Studies estimate that 6–27% of women worldwide suffer from chronic pelvic
pain. Because it can be complex, successful management usually involves a
multidisciplinary approach (medication, therapy, physical therapy, etc.) tailored to each
woman.
● Uterine Fibroids: Fibroids are benign (non-cancerous) tumors that grow in the wall of
the uterusThey are very common – up to 80% of women have fibroids by menopause –
though many have no symptoms. When fibroids do cause problems, women may
experience heavy menstrual bleeding, pelvic pain or pressure. Large fibroids can press
on the bladder or bowel, leading to urinary frequency or constipationTreatments range
from medication to minimally invasive procedures, depending on symptoms and goals.
Each of the above issues is common in women’s health and highlights why paying attention
to pelvic symptoms is so important. Future posts in this series will explore these topics in
depth, but first it’s key to recognize them and know that effective care is available.
Early Detection and Open Conversation
Early diagnosis and regular gynecologic care are vital for pelvic health. Women’s health
providers are trained to evaluate pelvic concerns. During a routine exam, your provider can
check for issues or recommend tests (like pelvic ultrasound) and treatments (such as pelvic floor
physical therapy) if needed If you notice any changes – for example, new pelvic pain, unusual
pressure, or bladder/bowel leaks – do not hesitate to mention them. Many women feel
embarrassed to bring up pelvic symptoms or think they are “just normal,” but that silence can
delay help
Remember that urinary incontinence and pelvic pressure are not “normal” parts of aging,
and there is nothing shameful about seeking help. Talking openly with your doctor can lead
to earlier, less invasive treatments. In fact, learning about the pelvic floor can help you spot
problems early. Being informed makes you an active partner in your care. Regular checkups
also allow your provider to address other aspects of pelvic health (for example, discussing
pelvic floor exercises, lifestyle changes, or preventive screenings). In short, don’t wait to speak
up – early action can make pelvic conditions much easier to manage.
Ready to Take the Next Step?
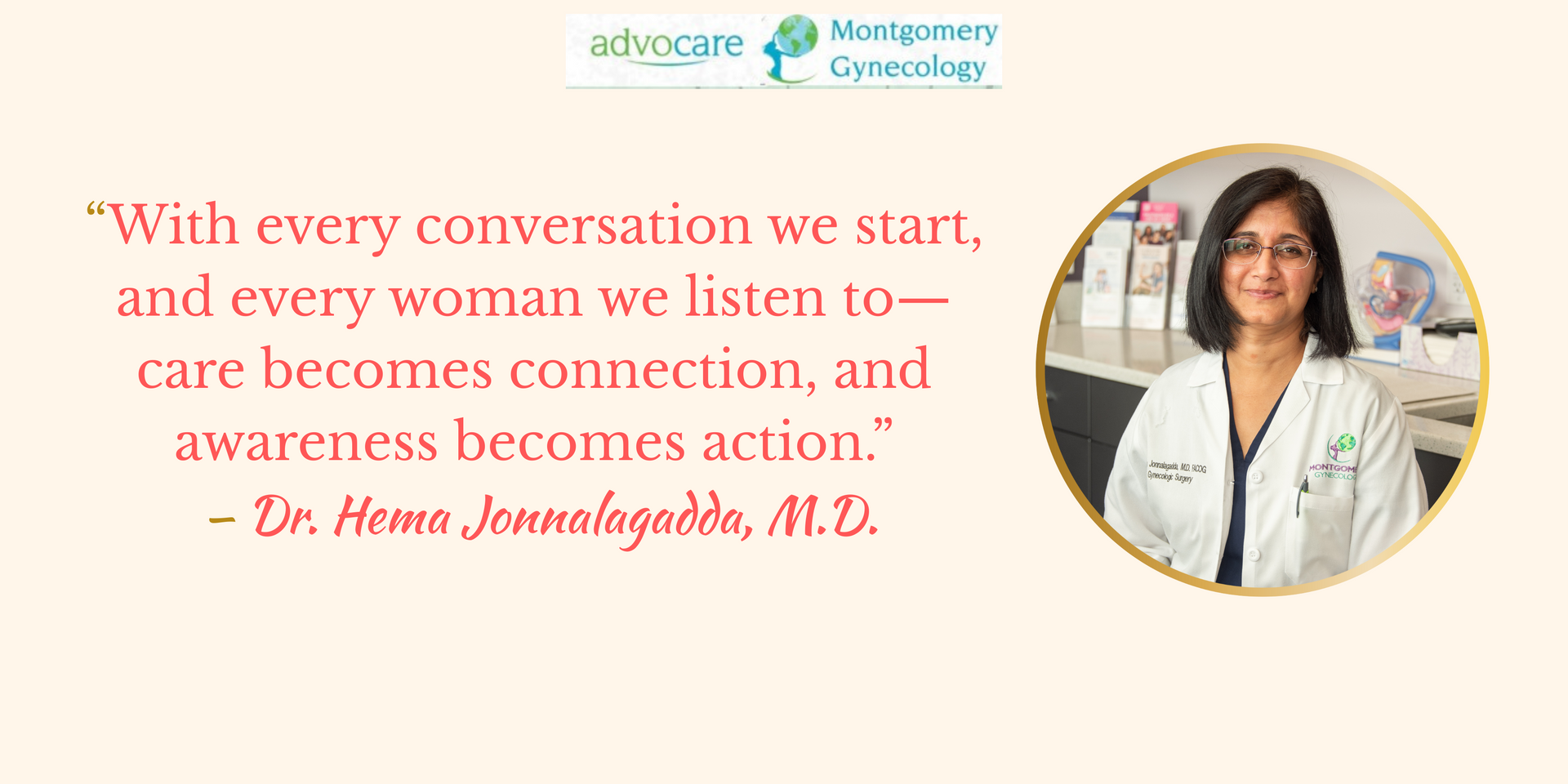
Dr. Hema Jonnalagadda and the team at Advocare Montgomery Gynecology are committed to
providing compassionate, expert care for all aspects of women’s pelvic health.
If you’re experiencing symptoms or simply want to stay proactive, we’re here to help.
👉 Visit our practice page to learn more or book an appointment today.
Your pelvic health matters—and you don’t have to navigate it alone.